
Have you ever found yourself in a group of new friends and pushed yourself a little (or a lot) because you didn’t want to bring up your diagnosis? Have you ever felt anxious about going to your cardiology appointment and thought “I could put this off for another few months?” You are not alone.
There are a number of reasons people avoid seeing their cardiologist: not having specialist healthcare centres close enough to where you live, inadequate health insurance, not receiving the right information about your condition at the right time, or maybe you’ve had a bad experience with your doctor/nurse/hospital and are hesitant about going back.
In addition to these, I think there is an important factor that is even less talked about.
Adolescence and Chronic Illness
Adolescence and young adulthood is a time of transition. Our bodies change. Also, the way others relate to us and the way we think of ourselves changes. We may start to want more independence from family and begin to make more choices for ourselves. Our friends and peers become more influential in our lives, whether we like it or not.
Going through this transitional time as a person with chronic illness(es) adds another complicated layer to this period in our lives which is already characterized by change, instability, and exploration. Having a chronic illness means that in addition to going through the usual developmental milestones of adolescence, we are also learning to understand and manage the physical, emotional, psychological, and social consequences of our disorder.
Our bodies are the vehicle for how we interact with our world and how other people interact with us. We learn to make sense of ourselves and our bodies based on these interactions.
We also live in a society where health is privileged. Our world, our work, our schools, our transportation, our grocery centers, our parks (I could go on and on) are mostly organized for healthy people. When we are sick or live with a chronic illness these ableist structures can remind us that we are not the norm.
There are times in our lives where we might feel this more intensely and I would argue that adolescence is one of them. As adults, with the perspective of hindsight, we might push back or reclaim our uniqueness as people with Marfan syndrome. It does not mean we don’t still feel it though.
Becoming Aware
As a young girl growing up with Marfan syndrome, I think I only began to be aware of my disorder (apart from the many doctor visits) when I had my first heart surgery at 10 years old. My mitral valve needed immediate attention. Months after surgery I remember laying on the floor playing Barbies with my sister because when I sat up I would get dizzy and my heart would race. No post-complication would not stop me from making sure Barbie attended high school.
Two years later I had an aortic root replacement but because I felt physically okay at the time, I was mostly upset at the idea of missing out on the grade 7 drama. I am lucky enough to have a family who took on the responsibility of managing my care so I could focus on important child-like business – like convincing them I had to have a dog, play hopscotch, and ride my bike with my sister and friends. I do not recall understanding or questioning why I felt so fundamentally different; I only knew that I was.
As I grew older I become increasingly more aware of the intricacies of my condition. Some of this was likely due to taking on aspects of my own care and some was from watching how the decisions, fears, consequences, and symptoms I lived with were so different from my peers.
For example, when I was 17 I underwent a spinal fusion. That surgery was my choice, in consultation with my orthopedic surgeon and family. It meant missing out on the end of grade 11, my friend’s prom, and other summer activities. It also meant months of horrendous pain, isolation, and some long term consequences for the trade-off of having a straighter spine. This decision was in line with my mantra at the time: “I just want to be normal like everybody else.”
Identity and Marfan
As a teenager and young adult, this was accompanied with attempting to understand how living with Marfan syndrome fit into my identity. On the one hand, I wanted to feel comfortable and able to accept my condition as a part of who I was/am, instead of constantly having to worry about how to conceal it or when to reveal it. On the other hand, I felt the pull to reject and camouflage my diagnosis, despite how much it showed, in an attempt to fit in with society’s standards because it made/makes me feel different and flawed.
These feelings contributed to behaviour I am not proud of. Making risky decisions. Finding myself in dangerous situations. Spending time with people who were not concerned for my well-being. Harming myself and my body. Pushing away the people who truly cared about me because I felt profoundly misunderstood.
Some people say this is a phase that many kids go through, but it was more than that. I had a deep set anger, sadness and shame that I could not articulate at the time. Instead I tried to escape. I was desperately seeking loss of inhibition, approval and self-worth.
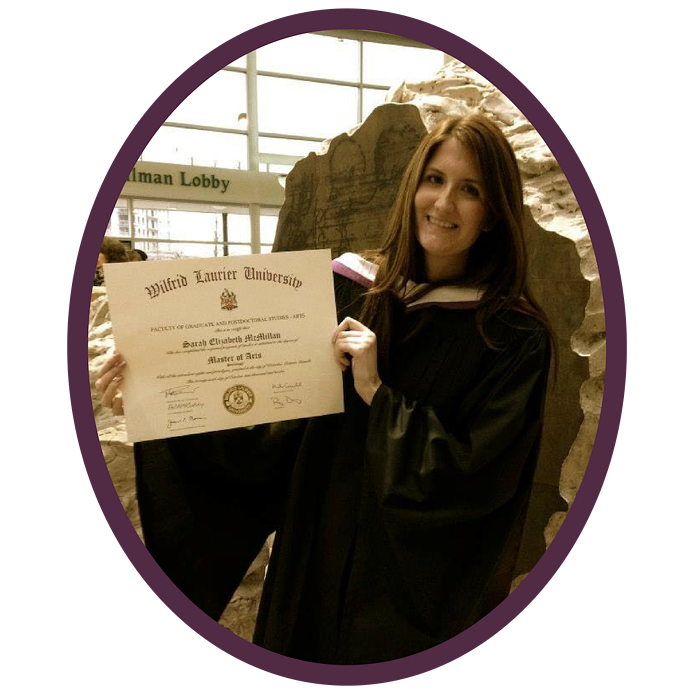
What I did not know until I began my undergrad and Master’s degrees in Sociology where I chose to research chronic illness, disability and Marfan syndrome, is that the way I was feeling and the behaviors I engaged in are common passive coping strategies experienced by young people with various chronic illnesses[iii].
I was simultaneously comforted and outraged by this information. People research and write about this stuff? Why did I not know about this? What do we as a community need to think and do differently to help our young people?
This leads to the area where I think we can improve – how we think and talk about acceptance, specifically as it relates to Marfan syndrome awareness.
Acceptance and Marfan
There were many moments in my life where I was not ready, willing or able to “accept” my diagnosis for the reasons I listed above. As a young adult, when I tentatively turned to professionals and patient groups for support and understanding I was met with the sentiment that – for my own good – I had to accept my diagnosis.
I thought, “How can I accept something as a part of who I am when my social world views it as undesirable?” These moments could have been opportunities for discussion about what it means to me to live with Marfan syndrome and what acceptance of my diagnosis could look and feel like. This kind of discussion may have brought me closer, rather than pushing me further away.
I don’t know for sure, but perhaps the motivating factor behind that push toward self- acceptance was related to concerns for my physical health. If you have Marfan syndrome you’ve hopefully heard that medical care and monitoring, specifically of the cardiovascular system, is central to lifelong management of this disorder. In that light, it’s logical that the people in our lives who hold caring roles would want to ensure we get the care we need to survive.
But as an adolescent and young adult, it was hard for me to understand what was driving their insistence. Indeed, this problem is undoubtedly related to a critique I’ve heard from other people with Marfan syndrome and felt myself – that the focus of Marfan syndrome care and research has been so intensely on keeping us alive (and for that we are grateful), but less so on what quality of life looks like and how to improve it. Thankfully I think that is beginning to change as there is a recognition that we need both.
We Need Both
In a similar vein, it is entirely possible to feel confused, uneasy, angry and a million other thoughts and feelings related to how your diagnosis fits with who you are. And yet, you should still continue to seek the follow up medical care you require.
At the end of the day, you do not have to accept your diagnosis, fully or in part, to be aware that your diagnosis can have deadly consequences.
So if you are a young person and can relate to any of this, I want you to know – I see you. Heck, if you’re an adult and you’re feeling this way too, you are not alone. There are many possibilities for living well with Marfan syndrome. My hope is that through continued conversation and awareness of a varied kind you will find what fits best for you.
The Foundation offers many opportunities to connect with other people who are on the same medical journey as you are. These include local Walks for Victory, our annual conference every summer, and regional symposium. We can also connect you with an individual mentor.
A Canadian study of adults with complex congenital heart disease tells us that 27 percent of patients over the age of 18 had not engaged in further cardiology visits[i]. A similar study surveyed over 900 adults with congenital heart disease across the United States. They found that 42% of patients had a 3 years or longer gap in cardiology care and that the average time where their first gap in care occurred was at 19 years of age[ii]. They also tell us that the majority of people who responded to the survey were aware of their heart condition.
[i] Pauliks, L. B. (2013). Depression in adults with congenital heart disease-public health challenge in a rapidly expanding new patient population. World J Cardiol, 5(6), 186-195. doi:10.4330/wjc.v5.i6.186
[ii] Gurvitz, M., et al. (2013). “Prevalence and predictors of gaps in care among adult congenital heart disease patients: HEART-ACHD (The Health, Education, and Access Research Trial).” J Am Coll Cardiol 61(21): 2180-2184.
[iii] Lambert, V. and D. Keogh (2015). “Striving to live a normal life: a review of children and young people’s experience of feeling different when living with a long term condition.” J Pediatr Nurs 30(1): 63-77.

Sarah, who has Marfan, is a research associate, social worker, and qualifying holistic practitioner who lives in Toronto, Canada. Over the years she has used different styles of writing and research as a therapeutic tool for learning to live well with illness. She has her diagnosis to thank for directly shaping her desire to improve health systems and experiences of illness.
