
CAUTION: This story focuses on a detailed account of fatal childhood aortic dissection; the story is shared to save lives through increased awareness.
“I will always wonder if there would have been a better outcome if the doctors at the hospital would have known about VEDS.”
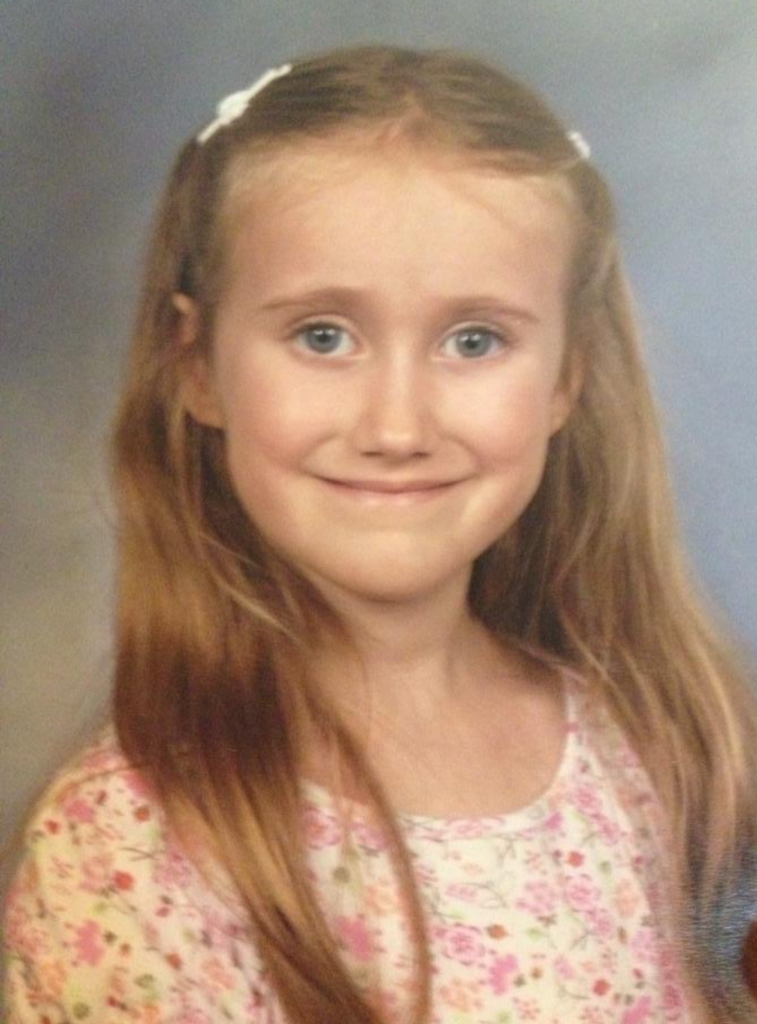
Jenny Paquette of Florida, whose 12-year-old daughter – Natalie – lost her life due to aortic dissection as a result of undiagnosed Vascular Ehlers-Danlos Syndrome (VEDS), still thinks about what might have been, 9 years after her daughter’s tragic passing.
“Natalie was fine during the day. One night, she was in the bathroom – we were visiting some relatives. She was in there for a long time. She came out and said, ‘Mommy, I can’t feel my leg, and my back hurts.’ At first, I thought her leg was asleep. She was lying down and just didn’t seem right.”
When Jenny saw that her daughter’s leg was not only numb but also “completely white,” she called 911. From the beginning, given that Natalie was a healthy, active child who played basketball and soccer and was a dancer, first responders, and healthcare providers did not recognize the signs of aortic dissection and VEDS.
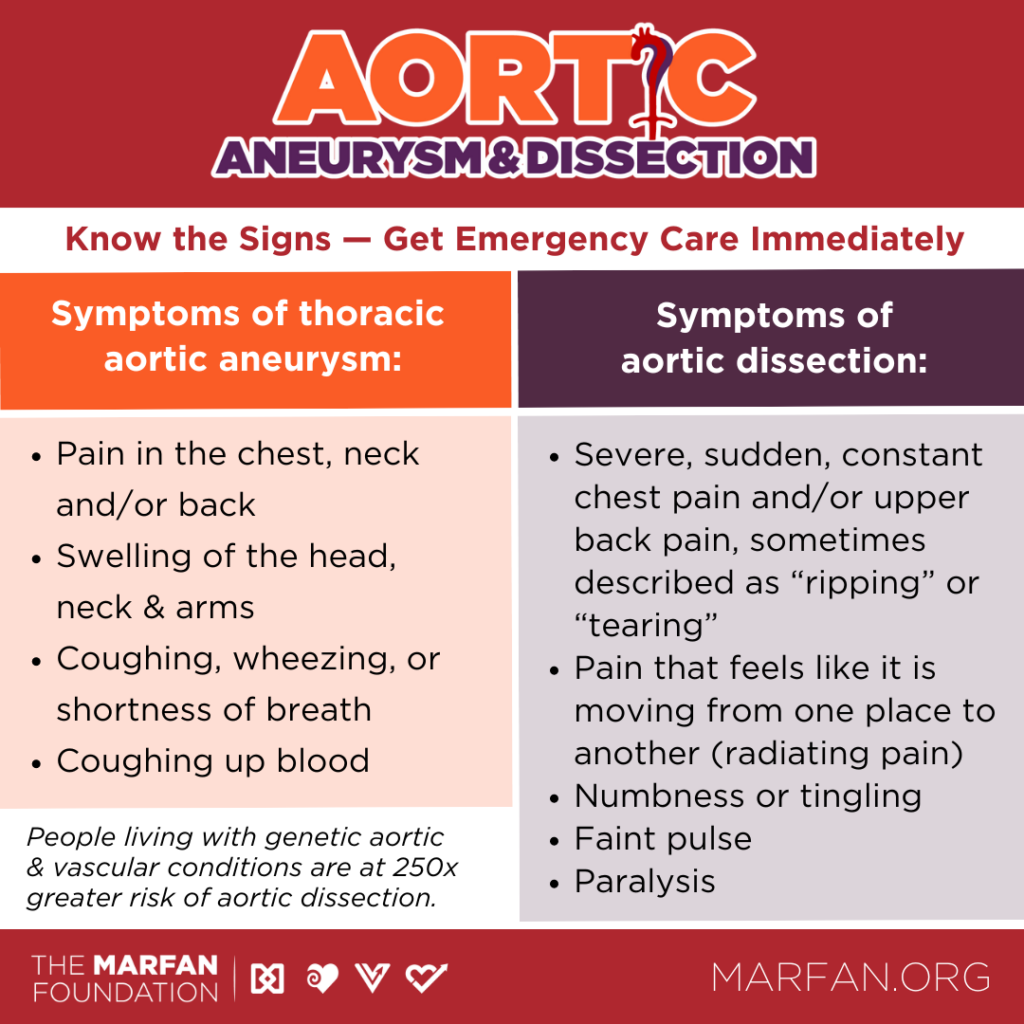
Because Natalie’s heart rate was mainly stable initially, first responders bypassed a hospital ten minutes away and instead took Natalie to a children’s hospital 45 minutes away, unknowingly delaying crucial emergency treatment. Aortic dissection is typically diagnosed via a stat CT scan and treated via immediate surgery. Because of Natalie’s age, the first responders did not use lights nor sirens, trying to make an ambulance ride less stressful for a child nobody dreamed was experiencing a life-threatening aortic emergency.
Jenny was asked if her daughter could have gotten into something in the medicine cabinet. At the hospital, Natalie – who was not yet menstruating – was given a pregnancy test.
“They were just grasping at straws. They had no idea what to look for,” said Jenny. “It’s so important to spread awareness, and the doctors need to be more knowledgeable,” said Jenny.
At the hospital, Natalie was going in and out of consciousness – even then, Jenny didn’t fully realize the gravity of her daughter’s condition, nor did healthcare providers as precious life-saving time continued to pass. Jenny thought perhaps Natalie was so scared she was simply falling asleep and waking back up here and there. An IV was put in – it “popped out.”
“It took forever to get it back in. It took forever to call a cardiologist [as more serious symptoms began to develop],” said Jenny. “I went to the bathroom, and I came back. I heard one of the nurses say, ‘She’s extremely tachycardic,’ and I ran in [to Natalie’s side],” said Jenny.
Once the cardiologist had figured out that Natalie’s aorta was the reason for her worsening symptoms, he pulled Jenny aside and told her Natalie was not likely to survive.
“I said, ‘No, she’s not going to die.’ I just didn’t believe him. I thought they were telling me the worst-case scenario,” said Jenny. Doctors planned to fly Natalie to Tampa General Hospital for emergency surgery – telling Jenny they’d “never seen this in a child.” The helicopter experienced a mechanical breakdown, and the flight never happened.
Jenny was talking to her brother by phone, ironically a vascular surgeon, when Natalie took a final turn for the worse.
“I heard them calling for help. I dropped the phone and ran in. They were doing CPR.” Four hours after the onset of symptoms, Natalie was gone. Healthcare providers learned that Natalie had VEDS post-mortem.
“She was just the sweetest person that I’ve ever known in my life because she never said anything harmful about anyone,” said Jenny of her daughter. “She was a very brave little child. Riding roller coasters. Going up on stage and singing songs in front of her whole school. She stood out to me as being brave, generous, and exceptional. I always felt that about her, even before she passed — she was just like an angel.”
Jenny, a believer in frequent pediatric care, had never been told Natalie was anything but “perfectly fine” throughout her child’s all-too-short lifetime. “We’d never even heard of VEDS before.”
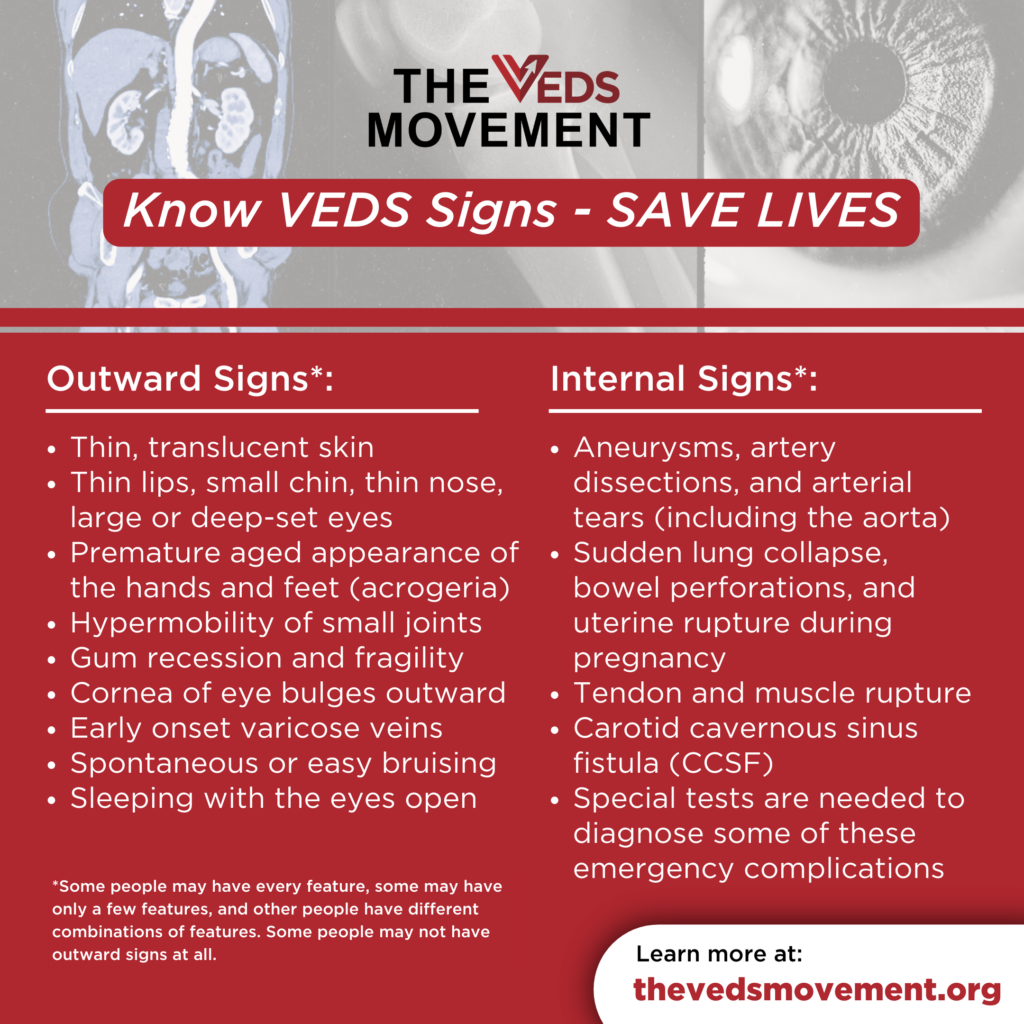
After learning much more about VEDS following her child’s passing, Jenny said there were a few small signs of VEDS present: some typical VEDS facial features – most noticeable in Natalie’s youngest years; easy bruising – which doctors had chalked up to usual childhood playground injuries when Jenny asked; and gastrointestinal issues. Natalie was tested for anemia due to the bruising, and when those tests came back normal, providers “kind of blew that off,” said Jenny.
Jenny wants to spare other families the pain and grief she and Natalie’s whole family have experienced by raising awareness of VEDS and aortic dissection. Natalie, like about half of people with VEDS, appears to have carried a “spontaneous” mutation of the COL3A1 gene that caused her to have VEDS. In contrast, half of people with VEDS inherit the genetic mutation. None of Natalie’s family members who had genetic testing have VEDS – including Jenny.
80% of people living with VEDS will experience sometimes fatal vascular complications by age 40. Experts estimate that 1 in 50,000 to 1 in 200,000 people are living with VEDS. Many are undiagnosed.
Signs of VEDS can entail unexplained easy bruising, an aged appearance of the hands, and a distinctive facial appearance, which may include thin lips, a small chin, a thin nose, and large or deep-set eyes. Signs of aortic dissection may include severe, sudden, constant chest pain and/or upper back pain, sometimes described as ripping or tearing; pain that feels like it is moving from one place to another; unusually pale skin like Natalie’s white leg; a faint pulse; numbness or tingling; paralysis; and in some instances, there may be no pain but a sense that there is something terribly “wrong.”
Jenny hopes that Natalie’s legacy may include the purpose of saving other young people’s lives.
“I would feel like it was something that Natalie has helped with, or it would be honoring her to spread awareness — and for more people to know. If we could just save more lives, that would be incredible…amazing.”
For media inquiries, please contact April Dawn Shinske at brandcomms@marfan.org.

April Dawn Shinske is the Chief Communications and Marketing Officer for The Marfan Foundation. She is proud to lead a stellar integrated marketing and communications team and honored to help tell the amazing stories of our community members.
